This Open Enrollment White Paper Includes the Following
Table of Contents:
- ABSTRACT
- EARLY PREPARATION
- ESTABLISH AND FOLLOW A TIMELINE
- PROVIDE CLEAR COMMUNICATION
- AVOID DELAYS DURING ENROLLMENT
- POST ENROLLMENT FOLLOW UP
- CONCLUSION
Abstract
At Providence Technology Solutions, we are here to help you embrace the challenges and look at open enrollment season not as a chaotic time of year, but as an opportunity to deliver exceptional service. We are committed to helping you manage your benefits platform and to support and engage your employees and staff. Open enrollment guidance and support is just one of the many quality, affordable services we can provide. This, along with our expertise and advice, will help support you and your employees with a positive open enrollment experience.
One of the most stressful times for a company and HR professionals is the period leading up to open enrollment (OE). Time spent preparing to modify the company’s benefit programs can be frustrating for employers and can often take the focus away from a company’s actual business for weeks at a time. Employees are also often overwhelmed with information and need assistance. Proper planning for open enrollment is essential to make the most out of available time and resources as well as to ensure a successful open enrollment season.
Early Preparation
Early preparation for open enrollment will help ease the burden for employers, HR Professionals, and employees. Preparation should start well before enrollment begins.
The first step, and perhaps the most important, is to look back at previous enrollment periods to determine what tasks were the most challenging and time consuming. By evaluating past processes, you can find ways to resolve these challenges and prepare for a smooth enrollment period.
Resources should be contacted and engaged early to ensure the workload is not carried by one person alone. Many employers work directly with Insurance Brokers who will generally contact you 3 – 6 months prior to your renewal to present you with the renewal package. If they do not reach out first, contact your Broker early and request for them to begin the process of gathering quotes especially if you want to look at other coverage or make changes to existing to plans. This will allow the Broker sufficient time to create a comprehensive renewal package with additional quotes and options for you to discuss. Selecting the best benefit offerings to provide to your employees can be a long process; however, early preparation can alleviate stressful last-minute decisions and changes.
Once you have selected your benefit offerings, you will need to consider how the cost will be divided between the company and your employees. These decisions are most often made in conjunction with your executives and/or board of directors. You will want to ensure these parties are part of the conversation as early as possible, and that their schedules are kept in consideration as well. Allow plenty of time for decision makers to review and compare contribution strategies. Schedule adequate time to finalize decisions and relay the new information to be included in employee documents and added to your enrollment systems.
All this information, as well as enrollment forms, plan summaries and benefit certificates obtained from your carriers should be included in packages provided to your employees. You may not know exactly how long it will take to create these packages, but it is important to plan how much time is needed for the tasks that are within your control.
Establish and Follow a Timeline
Establishing a defined timeline will support a cohesive plan of action to address the never-ending cycle of reviewing, analyzing and planning the next open enrollment period. Developing a clear plan of attack is key to being successful.
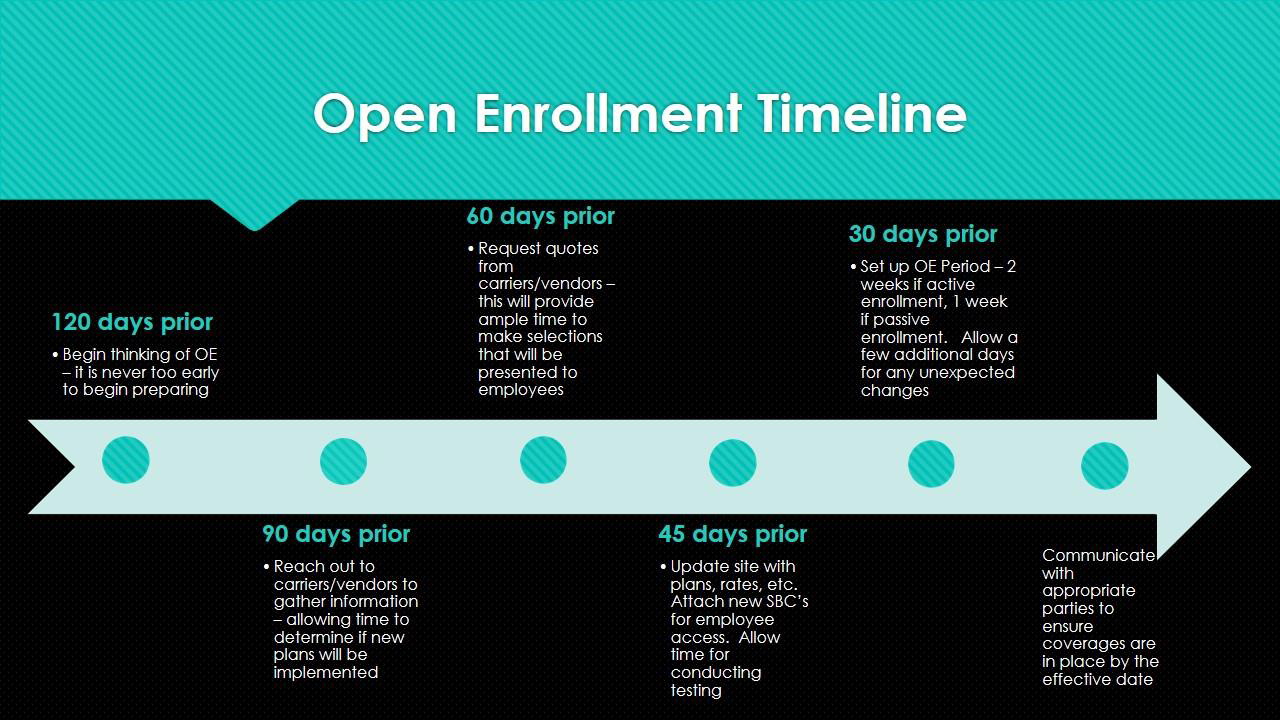
It is never too early to start planning when it comes to an open enrollment. Preparing well in advance is key so staying in touch and working with your Brokers or providers throughout the year will provide significant assistance in this decision process. You should begin as early as possible the process of reviewing the existing benefits package to determine whether any new plans should be offered. There should be an absolute minimum allowance of 120 days to begin these conversations with the Broker and insurance carriers. Working closely with them can help to improve and eliminate any issues that may occur during the process.
This will allow for use of the next 60-day period to choose the appropriate plans, as well as provide the essential time to update your HR Software with any relevant data or functionality such as new plans, dates, plan documents, and rates. In addition, it is important to provide ample time to review, conduct testing, and make any updates to the employee benefit and open enrollment guides if necessary.
Consider your enrollment options and ward off procrastination by providing concise OE period dates, clear deadlines and provide frequent reminders to employees accordingly. If employees are required to re-enroll (active enrollment), you may want to allow for a longer enrollment window (suggested maximum of 14 days). If the prior year benefits carry forward to the new plan year (passive enrollment), the length of time can be shortened (5 to 7 days) to allow for any election changes. Below is a helpful graphic you can reference to assist with planning efforts.
Communication with your personnel is crucial and should be done early and often. Especially if there are plan changes, communicate early and often with any personnel impacted. Providing the adequate time to communicate announcements and reminders to your employees to review the options and make their elections, best supports a stress-free enrollment period.
Remember to include a minimum of 5 days after the enrollment period ends to allow for administrative review. This additional time allows you to capture and analyze demographic data for employees and their dependents such as missing social security numbers, required dependent verification documents, and full-time student status confirmations. It will also provide the necessary time for your employees to review their confirmation statements and make any adjustments or updates accordingly. Once the statements are confirmed, review and compare the elections to the previous year, noting any changes that will require starting or removing future payroll deductions. This administrative review period is best practice to ensure that the appropriate parties have been notified, coverages are in place by their effective date, and allow for any unexpected changes that may occur.
Once enrollment ends, start planning for next year. Survey your employees about their experience and implement any feedback to adjust your strategy for next year. Making proactive adjustments will aid in alleviating confusion and stress during future open enrollments for both the employee and employer’s experience.
Provide Clear Communication
Throughout open enrollment you want to ensure you follow your prepared timing strategy and stay organized. Organization not only refers to tracking your goals and deadlines, but it also includes keeping your notes and communication organized. Working with an electronic platform may make the overall process easier, but you also need to ensure you are keeping your employees informed. The value of proactive and transparent dialogue is often overlooked.
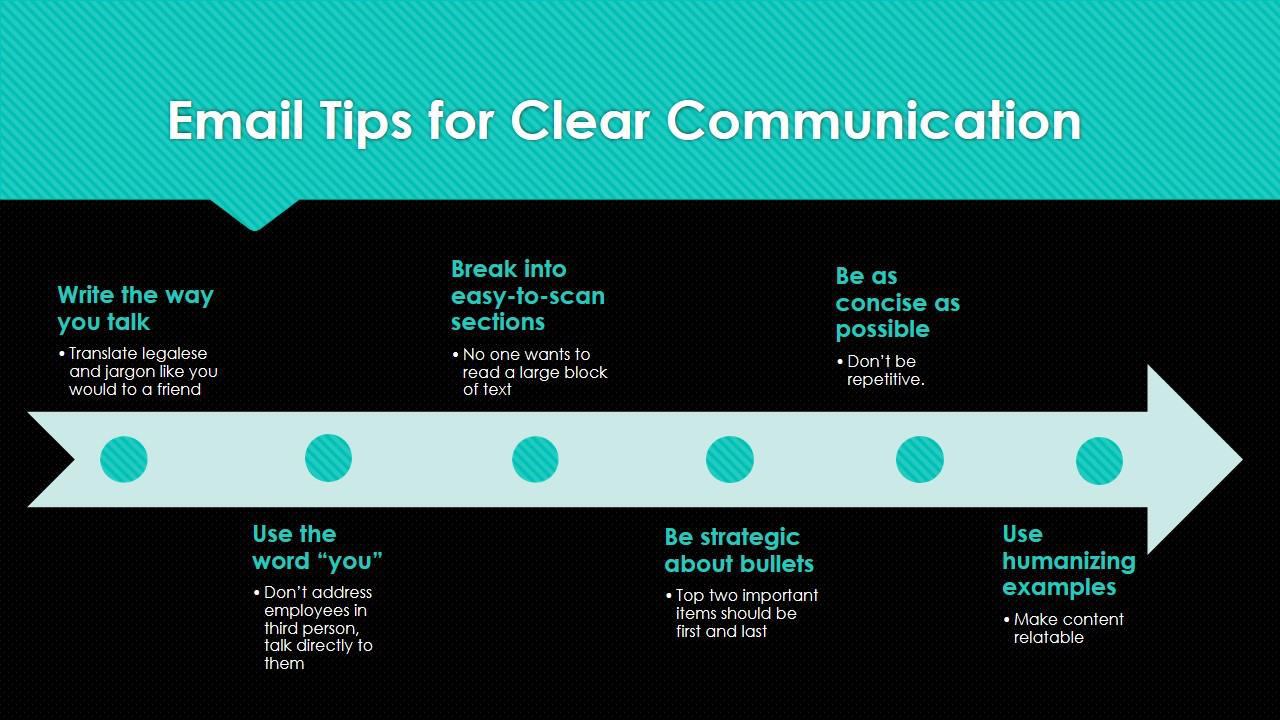
In this digital age, it has never been easier to reach out to employees throughout the open enrollment process. Email is literally at our fingertips, but one must be careful to use it wisely. Employees tend to view company emails the same way many of us react to reading personal communication that is too lengthy. We want our questions answered quickly and clearly. There are six tips to consider when creating open enrollment emails.
Another way to quickly get information to employees is through the use of text messaging. SMS messages are received instantaneously and are more likely to be read right away. You can send a short message with a reminder of when open enrollment meetings are or even when your system is open for enrollment. Similar to emails, you do not want to send lengthy messages. Additional or more involved information would best be left to attachments or physical handouts.
While electronic messages are quick and easy, you do not want to overlook the benefit of printed materials. Well-designed posters are an eye-catching way to deliver key points about open enrollment. Posters, like emails, should not include busy graphics or a lot of text, but instead use bright colors, simple images and bold text. A good example could be a vivid poster in the employee lobby reminding employees to review their current benefits ahead of the stated open enrollment period. A bright poster hanging in employee lunchrooms stating the location and time details of an upcoming open enrollment meeting.
Allowing enough time for employees to review all documentation and plans before the end of the open enrollment period is essential for reducing stress and increasing participation. Once the final decisions have been made, ensure employees have access to the proper forms, carrier links, provider directories and other pertinent information as soon as possible. If your enrollment will be done using paper forms, have an enrollment packet printed up and distributed to each eligible employee. For online enrollments, post all data in an easily accessible area of your site for employee viewing. Allowing for employees to review and complete the forms without feeling rushed, or online, will save time overall and allow for a faster process.
When distributing information to your employees, you want to ensure they have every opportunity to gather the data they need in a timely fashion. Much like the distribution of materials mentioned above, you want to ensure your employees get to hear the information as well. Many employees prefer a face to face meeting to review documents, hear explanations of plans and changes, and can ask questions and receive immediate answers. During live enrollment sessions, ensure employees have access to the benefit documents either with handouts, printed benefit guides, or access to a computer during the meeting. For employees who may not be able to attend in person, record the meeting so they may listen later to benefit from any questions and answers discussed in the meeting.
Whether your open enrollment is online or on paper, make sure you use a variety of online and offline options. Just as there are different types of learning preferences, there are communication preferences as well. Human Resource professionals who can communicate to, and with, their team members in a clear manner can alleviate stress on both sides and permit the process to run smoothly and efficiently. Remember, communication is not only between you and your employees, but between your Brokers and vendors as well. Reaching out to and following up with your outside contacts is imperative to receive necessary information to relay to employees. Once open enrollment is complete, you will also need to gather the enrollment information to send back to vendors, ensuring all details are processed correctly and timely allowing employees to use their new benefits on the effective date. Preparation, following a timeline, and communicating well are all keys to avoiding delays throughout your open enrollment process.
Avoid Delays During Enrollment
Online enrollment systems make the benefit election process more efficient by providing 24/7 access to review or change benefit elections. However, to reduce errors and delays you want to make sure your systems are thoroughly tested and audited prior to opening the enrollment period for employee access. One small discrepancy in the system can create setbacks, as corrections are made during enrollment, hindering the timely completion of the employees’ enrollments.
Testing your enrollment system involves reviewing the plans, rates, and documents, but also how the enrollment process flows. Include links to external sites and any required carrier forms as part of the online enrollment experience. If the process is not easy to manipulate or information is not clear, employees will reach out with additional questions postponing enrollment confirmation.
One of the most common requests from employees during an online enrollment is to reset their system password. Many employees only log in to the system once a year during open enrollment. Performing a one-time universal password reset at the beginning of your open enrollment period will eliminate this issue. Clearly communicating reminders of full login credentials and enrollment instructions will prevent your employees from being locked out and reduce initial stress and confusion. Some employees, no matter how much you remind them, will wait until the final day or in some cases, final hours, to complete their elections.
Employees can be encouraged to confirm enrollment early using incentives. One easy and cost-effective way is to use promotional items many carries have on hand. Carriers may have give-away items such as toothbrush kits, glass cleaners, stress balls and even mouse pads. You can offer these items as prizes for early enrollment. Activities such as these can add a stress-free element to enrollment, decrease delays and engage employees in the process.
Follow up with employees throughout the enrollment period, do not wait until the last day. Employees may look at the information at the start, but forget to go back and complete the enrollment. Monitor completed enrollments and send reminders to employees who have not yet finished their selections. The more the system is monitored during the process, fewer individual post-enrollment exceptions will be necessary.
Post-Enrollment Follow-Up
Just as it is important to review information before enrollment opens, it is imperative to examine data received once your enrollment closes. You will want to review election results to ensure all employees completed enrollment, contingencies were met, limits were not exceeded, and corresponding forms were completed and returned.
During the review, it may become necessary to make changes to an employee’s election due to an erroneous selection or requested modifications. Your vendors have their own deadlines for receiving completed information and correcting information after an initial file is sent to vendors is time consuming and frustrating for all involved. Make sure you factor in time for your review and the necessary changes before any data is sent along to carriers.
Once you have finalized the elections and forwarded it to the appropriate carriers, have confirmation statements available to each employee for their records. Electronic enrollment systems generally have an option to send individual statements in bulk at a designated time after enrollment. For paper enrollments, it may take a little more time and planning so take this into consideration as well.
After all data has been sent to employees and carriers, it is helpful to get feedback on how the process went for others. Meet with your team to discuss what they feel went well and what could have gone better. This is great information to have for next year when you begin planning all over again. Not only is peer review helpful, but surveying employees for their opinions can provide helpful insight into possible changes for the following open enrollment.
Conclusion
The perceived dreaded open enrollment period can become manageable and less hectic with a clear plan of attack. As indicated above, this would include early preparation, establishing and sticking to an aggressive timeline, and providing ample direction through clear communication, in addition to post-open enrollment follow up. Providence Technology Solutions has the expertise, knowledge and resources to provide superior service and guidance to embrace the challenges and to support you with a positive open enrollment experience. Contact us directly if you’d like to learn more.



